Cervical cancer a major public health concern
Andile Tshuma, Chronicle Reporter
ZIMBABWE this week marked cervical cancer screening and awareness week, with calls for more resources to be directed towards treatment of the disease.
In Zimbabwe, close to 2 000 women die every year from cervical cancer alone while 3 043 new cases are diagnosed. This is despite the fact that the disease is preventable and treatable if detected early.
The month of January was set aside to raise awareness and generate demand for the uptake of cervical cancer services. In Zimbabwe, cervical cancer screening is offered for free in most Government health facilities, but most women, including those with HIV, are not aware of the services.
Those that test positive sometimes fail to access treatment as it is not easily accessible, especially in rural areas.
Cervical cancer is a major public health concern with a disproportionately higher disease burden (84 percent of all cases and 87 percent deaths related to cervical cancer) in low-and middle-income countries.
For instance, the number of cervical cancer cases in Zimbabwe increased from 542 in 2008 to 1 368 in 2015. The sub-Saharan Africa region has an age-standardised incidence rate of 43 per 100 000 and a mortality rate of 20 compared with the global estimate of 14,0 and 6,8 respectively.
Among countries in southern Africa, Zimbabwe carries the highest burden, with an age-standardised incidence rate of 62 per 100 000 women, that is, an incidence rate five times higher than the global average. Furthermore, the age-standardised mortality rate of 46 per 100 000 women in Zimbabwe is nearly seven times the global average.
The 2018 estimates indicated that about 3 186 women were newly diagnosed with cervical cancer and 2 151 died due to cervical cancer in Zimbabwe.
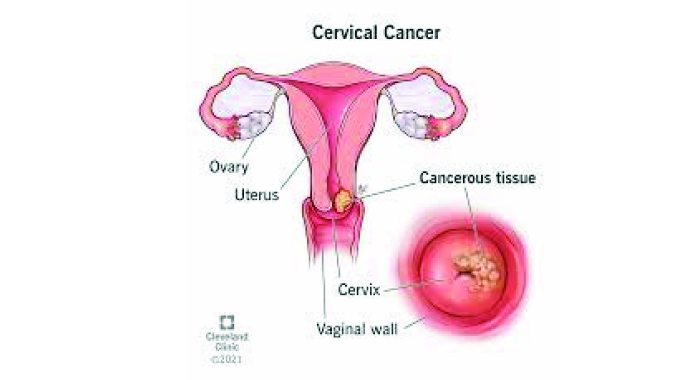
Cervical cancer develops in a woman’s cervix (the entrance to the uterus from the vagina). Almost all cervical cancer cases (99 percent) are linked to infection with high risk human papillomavirus (HPV), an extremely common virus transmitted through sexual contact. Although most infections with HPV resolve spontaneously and cause no symptoms, persistent infection can cause cervical cancer in women.
The introduction of the HPV vaccine into the country’s routine immunisation programme is expected to be a game changer in the country’s fight against cervical cancer, as Zimbabwe started vaccinating girls between the ages of 10 and 14 against cervical cancer in 2018. The move is expected to lower the incidence of cervical cancer in the coming years.
According to the Zimbabwe National Cancer Registry, cervical cancer leads among cancers in women, and constitutes 33,2 percent of the cancer burden in this population with more than 1 400 cases in 2020.
The World Cancer Research Fund adds that Zimbabwe has the fifth highest burden of cervical cancer in the world.
Over a thousand women die from the disease in the country every year, making it the most common cause of cancer deaths in women in the country.
Women living with HIV have a six-fold higher risk of cervical cancer than women without HIV, and cervical cancer is classified as an Aids-defining condition.

HIV- Image taken from Shutterstock
It is worrying that cervical cancer was the leading cause of death among all cancer deaths reported in the country in 2018.
According to the National Cancer Registry, a total of 2 743 cancer deaths comprising 1 248 (45,5 percent) males and 1 495 (54,5 percent) females were recorded in Harare, Chitungwiza and Bulawayo in 2018. The leading causes of the deaths were cervical cancer (13 percent), prostate (10 percent), breast (7 percent), oesophagus (7 percent), liver (7 percent), non-Hodgkin lymphoma (6 percent), stomach (5 percent), lung (5 percent), and colo-rectal (4 percent). The other cancers constituted 36 percent of the recorded deaths.

National Cancer Registry
What could be contributing to the high mortality among cervical cancer patients is the delayed detection of cases.
Out of the 3 535 cases with a known stage of disease at diagnosis, 2 813 (about 80 percent) were in stage 3 and 4.
A cancer stage describes the extent to which the cancer has spread in the body from where it first formed.
When cervical cancer is detected in Stage 3, it means it has spread to the lower third of the vulva and the pelvic wall. Sometimes it would have already caused kidney problems and affected the lymph nodes.
Stage 4 means the cancer has spread beyond the pelvis to the lining of the bladder, the rectum or has spread to other parts of the body. This stage is also called metastatic cancer, which happens when cancer cells spread through the lymphatic system or blood to form tumours in other parts of the body.
If the majority of women diagnosed with cervical cancer are already at this stage, it then makes sense why they account for the most deaths from any other form of cancer.
The World Health Assembly adopted the global strategy to accelerate the elimination of cervical cancer as a public health problem.
Countries are expected to reach the threshold of less than four cases of cervical cancer per 100 000 women per year for them to be classified in the elimination of cancer stage.

World Health Organisation (WHO)
The World Health Organisation has set up the 90-70-90 targets to be reached by 2030 and to be maintained.
This means that 90 percent of girls should be fully vaccinated with HPV vaccine by age 15, while 70 percent of women are screened with a high-performance test by age 35, and again by 45 years of age and 90 percent of women identified with cervical disease should receive treatment.











Comments