Maternal deaths decline at Mpilo

Thandeka Moyo-Ndlovu, Senior Health Reporter
TEN years ago, Mpilo Central Hospital, one of the major referral health facilities in the country, was regarded as a death trap largely because of the prevalence of maternal deaths.
Pregnancy was a risk factor for many women from the southern region who relied on the hospital for quality healthcare services.
However, following interventions by the Government and training of healthcare workers, Mpilo’s maternal mortality rate (MMR) has drastically gone down from 655 to 203 per 100 000 live births.
Mpilo records 20 to 30 deliveries daily with the number of women who die in the process of giving birth having gone down by 69 percent

Mpilo Central Hospital
Reducing maternal mortality is one of the major Sustainable Development Goals (SDGs) of the global health community.
The aim of the SDG 3 is to reduce the global maternal mortality ratio considerably by 2030.
Speaking to journalists in Kadoma on the performance of the Reproductive, Maternal, Newborn, Child and Adolescent Health (RMNCAH) Programme, the Ministry of Health and Child Care’s acting deputy director for reproductive health, Dr Mervyn Venge said Mpilo Central Hospital has performed better than all central hospitals in the country in terms of reducing maternal mortality.
He said while institutional maternal deaths have been on the increase since 2019, Mpilo has managed to reduce and maintain a low rate in the past 10 years.
“The rising of institutional maternal rate reflects a struggling health delivery system and this has been worsened by the pre and post-Covid-19 challenges. However, Mpilo of all the central hospitals has maintained a decrease in maternal deaths compared to the past 10 years,” said Dr Venge.
“This is very commendable as our vision is to ensure all pregnancies do not cause a threat to the lives of women and newborn babies. We would like to commend Mpilo staff for the job well done.”
Dr Venge commended the country’s health care workers for continuing to work harder despite challenges revolving around staff attrition, low morale and burnout.
Commenting on the 10-year Mpilo study which was recently published in the World Journal of Perinatal Medicine by the acting chief executive officer Professor Solwayo Ngwenya, Dr Venge said the decline is a good sign of improved services at the public institution.

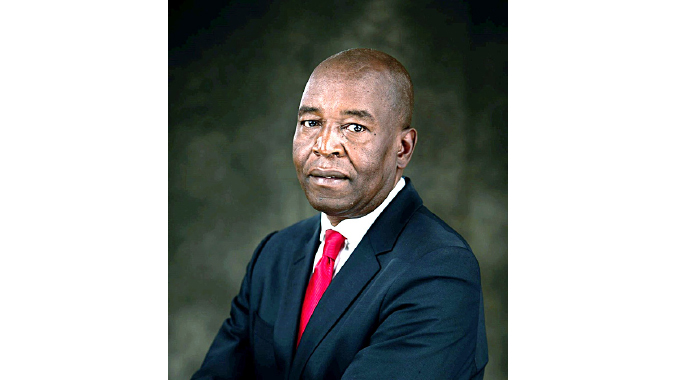
Dr Mervyn Venge
He said the reduction in maternal deaths is a great move towards ensuring members of the public from Bulawayo, Matabeleland North, Matabeleland South, Midlands and Masvingo provinces access quality healthcare services from a public hospital.
“The maternal mortality ratio (MMR) declined from 655 per 100 000 live births in 2011 to 203 per 100 000 live births by 2020. The commonest groups of maternal mortality during the period 2011-2020 were hypertensive disorders, obstetric haemorrhage, pregnancy-related infection and pregnancies with abortive outcomes,” read the report.
Haemorrhage which is an acute loss of blood from a damaged blood vessel, accounted for a majority of the maternal deaths countrywide. The Government had to scrap user fees for blood at all public institutions to address the issue of deaths.
“There were 273 maternal deaths recorded in the period 2011 to 2015 and 168 maternal deaths in the period 2016-2020. There was also a decline in maternal deaths due to obstetric haemorrhage,” said Dr Venge.
“Maternal deaths due to pregnancy-related infection also declined from 46 to 22 as well as pregnancies which end in abortion.”

HIV and Aids
Prof Ngwenya attributed the milestone to the introduction of Government interventions such as malaria control, the adoption of life-long Option B+ antiretroviral treatment for HIV-positive pregnant women.
“The Government also helped in the training courses of staff and the introduction of strong clinical leadership and accountability were all associated with a significant decline in the causes of maternal deaths,” he said.
A programme specialist for the United Nations Population Fund said the decline recorded even at national level was commendable.
“If we look at Maternal Mortality Ratio according to census data overtime, we note that it peaked in 2002 at 1 068 maternal deaths per 100 000 births. Since then, we have seen a steep decline because from 2002 to 2012, the Maternal Mortality Ratio declined to 525 Maternal Deaths per 100 000 live births,” said the specialist.
“Now, results which have been presented show that it has further declined to 363 Maternal Deaths per 100 000 indicating a six percent decline in Maternal Mortality Ratio.”
A total of 1 589 maternal deaths were reported during the same period in Zimbabwe against 437 478 live births, giving a maternal mortality ratio of 363 deaths per 100 000 live births.
The maternal mortality ratio was higher in rural areas at 402 deaths per 100 000 live births compared to 298 per 100 000 live births in urban areas. — @thamamoe











Comments