Tshelanyemba Hospital a ‘sick’ facility


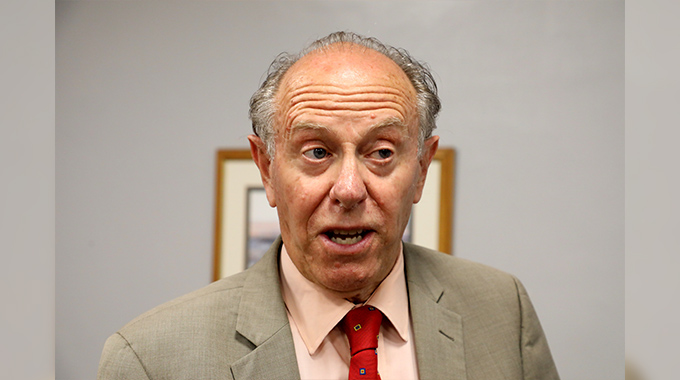
The president of the Matopos Rotary Club, Simon Moyo admires some of the goods donated to the Tshelanyemba Hospital by the Newfoundland Rotary Club in Canada
Nqobile Tshili Features Correspondent
Tshelanyemba Mission Hospital in rural Matobo District, Matabeleland South province, is itself a “sick” facility crying out for help. The Salvation Army Church-run health institution, which serves a community of about 70,000 people, is faced with a cocktail of problems. It is operating without a conventional ambulance while electricity and water are rarely available.
A rundown mini-bus has been operating as an ambulance for the past 15-years, experiencing frequent breakdowns on the bumpy, twisted and dusty 35km road linking the hospital with Maphisa. The Maphisa-Bulawayo highway, however, is in a good shape.
Gezile Zulu, 65, from Mazwi village lamented the ambulance challenge at Tshelanyemba Hospital.
The ferrying of critically ill relatives to either United Bulawayo Hospitals or Mpilo Central Hospital in Bulawayo in the absence of a reliable ambulance has become a hellish experience to people like her.
“The hospital itself needs healing. It’s in the intensive care. The unavailability of a reliable ambulance is forcing the hospital to detain patients who would have been referred to other hospitals.
“My father-in-law has been transferred to Mpilo Central Hospital but is still stuck at Tshelanyemba because the ambulance broke down. We can’t use public transport either because it’s risky and uncomfortable to a bed-ridden person. We are stranded and desperate. We urgently need assistance to take my father-in-law to Bulawayo,” she said.
Zulu cited the shortage of medical drugs as another burden that villagers have to contend with.
At times, senior citizens who are supposed to get free healthcare have to pay owing to the drug shortage at the hospital.
“We are largely a rural community. We don’t have any source of income and this affects us a lot. Sometimes we are told that there are no injections and we’ve to buy them. We sometimes leave the hospital untreated because of the drug shortage,” bemoaned Zulu.
To Winnie Dube of Nyashongwe Village, the biggest challenge facing the hospital is water shortage. This is especially so for expecting mothers.
Service delivery at the hospital and the health of staff and the community are greatly compromised due to the poor sanitation caused by water shortage, Dube said.
“Whenever there is no electricity the hospital will experience water shortages. There will be no water even for patients. This is one of many challenges affecting service delivery at our hospital. There is also the problem of inadequate food for patients. Patients need special diets to help them recover. We experience these challenges on an almost daily basis,” said Dube.
Tshelanyemba Hospital was forced to close last year as a result of an acute shortage of drugs, a development that affected thousands of villagers who were solely dependent on the institution for medication.It, however, opened later that year.
Hospital authorities point to the lengthy load-shedding periods as the reason behind the institution failing to pump water. The health institution uses the sand extraction method which needs power to produce water.
Tshelanyemba Hospital’s resident doctor, Dr Nyasha Muzilikazi, said an enhanced load shedding regime was affecting the operations of the hospital.
“Without water we can’t do anything. We bought a generator as a backup electricity source but it is expensive to run. We are serving a very small community and our cash inflows are very low. We have, as a result, to prioritise important issues,” said Dr Muzilikazi.
He said although they were facing a host of challenges, the hospital remained committed to offering quality health care services without compromise.
The hospital administrator, Major Tsaurai Mukwamuri, appealed to the corporate world and donor community to save the institution from total demise.
He listed the shortage of medical drugs and the hospital’s obsolete equipment as some of the biggest challenges that need urgent attention.
Major Mukwamuri said the hospital, just like any other health institution, was relying on the government grants, which sometimes, are released late.
He attributed the scant revenue base to the hospital serving a rural community where most locals have no ready source of income.
“We operate in a remote community where the majority of people are unemployed. They don’t have money to pay hospital bills and the cost of running the hospital becomes expensive,” he said.
Tshelanyemba Mission Hospital is a 103-bed facility which was established in 1923. The 70,000 population served by the hospital are from Bhewula, Kafusi, Sankonyani and Mazwi villages, among others.
Major Mukwamuri said the single kombi-turned-ambulance was overwhelmed by the hospital assignments.
He admits the ambulance has seen better days and should be off the road by now but there is nothing much that the hospital could do to replace it.
“We are using a kombi for an ambulance and this vehicle is 15 years old and it’s in a bad shape. We need a reliable ambulance as we at times experience complications when ferrying hospital supplies and patients. Our patients require to be transferred to other hospitals from time to time but we are handicapped,” said Major Mukwamuri.
Not all is gloomy at the Salvation Army Church-run hospital. Recently, the hospital received equipment to the tune of $100,000 courtesy of the Rotary Club of Newfound Land, Canada, working with Matopo Rotary Club.
The donated goods include mattresses, theatre beds, and an assortment of drugs. The hospital’s mattresses, just like most of the institution’s equipment, were now worn out.
There were fears that patients and visitors could end up infected by new diseases at the hospital.
Major Mukwamuri expressed gratitude to the Rotary Club for the donation. He said the donation would come in handy in improving the health delivery system.
Greg Peddle of St John North West Rotary Club in Canada said his club has been in contact with the remotely located hospital since 2007.
He said the challenges being experienced by the healthcare institution enhanced their commitment to improve it.
“This country is beautiful and has great potential. The hospital has a committed staff but they need our help. The administration and staff are pulling in the right direction. We’ve heard their concerns. We will look into how we are going to assist them improve their electricity generation. We are going to seek more funds so that the hospital can install solar,” said Peddle.
The president of Matopo’s Rotary Club, Simon Moyo, said his organisation was committed to assisting vulnerable groups in society.
Moyo said, funds permitting, the Rotarians would improve the hospital as well as uplift the standards of living for the surrounding communities.
The Matopo Rotary Club has initiated a mini-irrigation project for the hospital which is already bearing fruit.
Expectations are that the garden will produce excess vegetables to be sold to local communities at a commercial level.
Owing to the economic challenges faced by the country, the government has been releasing inadequate funds for the country’s hospitals.
In 2014 the Ministry of Health and Child Care submitted a budget of $712 million for the 2014 fiscal year but only received $337 million, inclusive of salaries.
The allocation received was 47 percent of the submission, signifying an 11,6 percent decrease from the 2013 allocation.
In 2015 the budget allocation for the Ministry of Health and Child Care further plunged to $301 million.
After the national 2015 budget was released, health experts predicted challenges for the country’s health care system. They said as the cost of living continued to increase, the poor will increasingly fail to access medication.
Access to health care is a fundamental human right that everyone is entitled to. According to the World Health Organisation (WHO) the right to health includes access to timely, acceptable, and affordable health care of appropriate quality.
This, however, is not always the case in developing nations as financial challenges coupled with economic sanctions, in the case of Zimbabwe, have made it difficult for Third World people to access quality health care facilities.
Many health institutions in rural Zimbabwe are a mirror reflection of Tshelanyemba Mission Hospital. They are in a sorry state as they barely have adequate resources.
According to World Health Organisation (WHO) the country maternal mortality is staggered at 614 deaths per 100,000 live births. This proves that the country has a lot to do in as far as providing health care provision is concerned.
The Deputy Minister of Health and Child Care Aldrin Musiiwa, said the government is aware of the challenges faced by hospitals but is incapacitated to deal with all of them.
“It’s not government policy that pregnant women should bring their items when they come for delivery at referral hospitals but at the moment, because of the economic crunch we are facing, we are running short of essential items which are to be used during delivery. Hence, the women have to supply. However, the government policy is that women should receive assistance at the hospitals without bringing any additional items for their treatment,” he said.











Comments